About us | Ko wai matou
Tu Whakaruruhau, Auckland Wellbeing Collaborative is a partnership of social service agencies who have joined up to support the implementation of a new model in primary care across Auckland.
The collaborative is made up of Maori and Pacific community organisations, Health NZ, primary health organisations, GP clinics, iwi and community health and social service providers.
Many providers are already part of the programme and more are being added every month.
This service is possible through government investment in wellbeing services, funded through the May 2019 Wellbeing Budget.
The collaborative is made up of Maori and Pacific community organisations, Health NZ, primary health organisations, GP clinics, iwi and community health and social service providers.
Many providers are already part of the programme and more are being added every month.
This service is possible through government investment in wellbeing services, funded through the May 2019 Wellbeing Budget.
Our history | Matou Hitori
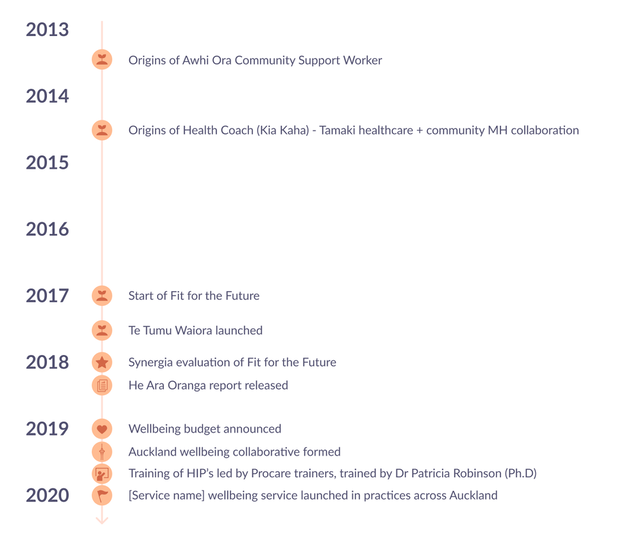
The three new roles - HIPs, Health Coaches and Awhi Ora Community Support Workers - make up the “integrated primary mental health and addiction” model of care.
The new roles were developed and tested in metro Auckland from 2013 and then brought together, piloted and evaluated in the the “Fit for the Future” initiative, during 2017/18.
The evaluation demonstrated the model was beneficial and in 2019 the Auckland Wellbeing Collaborative (Tū Whakaruruhau) formed to deliver the wellbeing model of service across Auckland.
The new roles were developed and tested in metro Auckland from 2013 and then brought together, piloted and evaluated in the the “Fit for the Future” initiative, during 2017/18.
The evaluation demonstrated the model was beneficial and in 2019 the Auckland Wellbeing Collaborative (Tū Whakaruruhau) formed to deliver the wellbeing model of service across Auckland.
Development of the wellbeing service
Pilot evaluation findings*
Access rates >90%
(compared to 30-50% under referral model).
Differential increased access
Maori, Pasifika, and young adult.
Good clinical outcomes
Significant reduced symptom scores, improved wellbeing; greatest improvement in Maori.
Reduced prescribing of psychotropic medications
Focus on prescribing only for severe persistent anxiety/depression
High level satisfaction levels with services
“How useful was this service today” average score above 9/10.
Significant increase in productivity
500-600 new patient/FTE/yr (vs 200-250/yr under package of talking therapy model).
*FIT FOR THE FUTURE: AN EVALUATION OVERVIEW FOR THE ENHANCED INTEGRATED PRACTICE TEAMS AND OUR HEALTH IN MIND STRATEGY

